The Health Consequences of Researching our Family and Community History
"In their fear, your forefathers gathered you too close together." Gibran Khalil Gibran
In 1992, I was thirty-nine years old, living in Sydney, Australia, when my father died in South Africa. I was heartbroken, as most migrants are with the loss of significant others overseas. I began dedicated research into my family history. Every week I faxed ten questions to my mother; for example: When and where was your father born? What was his education? What did he do when he first went to South Africa? After he’d married your mother, how did she feel about going to live in South Africa? Some of my mother’s answers ended up in my memoir, Olive Trees around my Table – Growing up Lebanese in the old South Africa.

At the same time, my father’s first cousin, Dr. H. I. Yazbek (Ivor) was drawing up a Yazbek family tree. He took us as far back as 1760.
We discussed Dr. Guita Hourani’s research of early Lebanese migration to South Africa: how the Maronite Church helped to establish the community despite the inhospitable British colonial government. Knowing this history strengthened us in the face of racism from white society. Nonetheless, early struggles left us with anxiety, fear of sickness and imperfection, and shame about our appearance, especially darker complexions.
In those times of racial classification based on skin colour, we were fearful of standing out and being noticed by the authorities, perhaps even losing our legally won white status with accompanying privilege. Having distaste for those manifestly different, some wore a reduced capacity for empathy, which had negative impacts on those who were ill or incapacitated.
Family History
Cousin Ivor had seen me on a few occasions when I was both well and unwell. Because of reticence about discussing health matters, the Lebanese being no exception, some of us, including an aunt of my father who had suffered similarly to me, were labelled hypochondriac. Cousin Ivor disputed this from a position of medical authority.
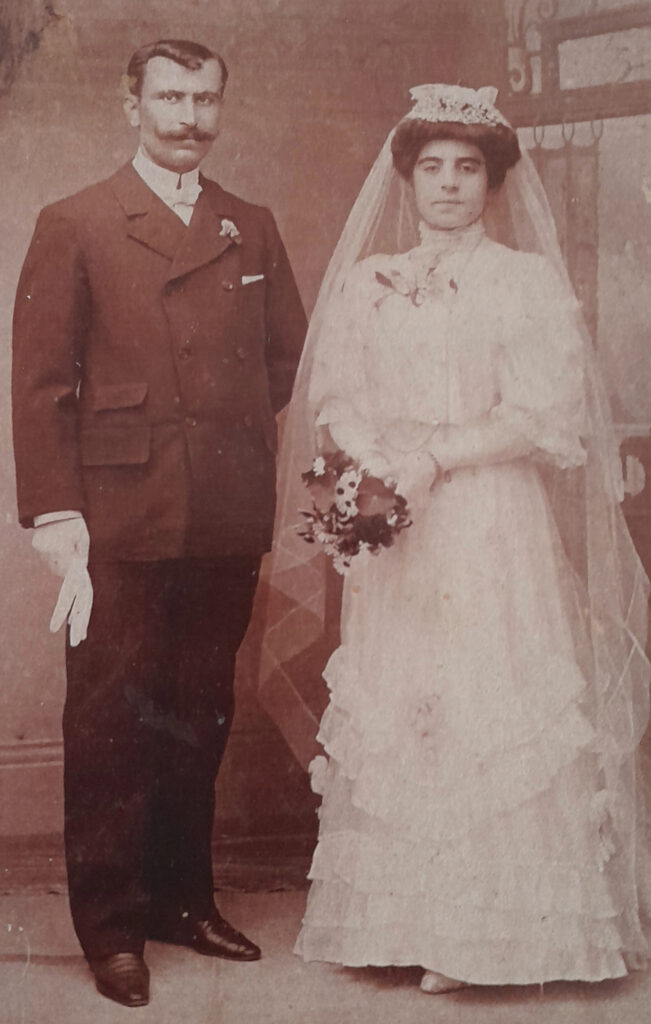
As my father’s general practitioner, he pointed out the consanguineous marriage of my paternal grandparents, his uncle and aunt: In 1907, my paternal great-grandfather was preparing to move to South Africa. His two older sons from his deceased first wife were already there, trying to start a business trading in ostrich feathers. His eldest daughter was eighteen and unmarried. Fearful of not finding a suitable Lebanese match for her in that distant and unknown place, he proposed a match with his brother’s son. The young married couple moved to South Africa with her parents, my great-grandfather and great-grandmother, where they had five children, one of whom became my father. At the same time, my great-grandparents had two more children, a total of ten Yazbek children from two wives.
Personal History
After years of serious illness with ambulance trips to emergency rooms and hospital stays for significant abdominal and joint pain accompanied by skin rashes and fevers measuring forty degrees Celsius, an astute doctor in Australia ordered a genetic test for me. This revealed that I had the gene mutations known as S108R and V26A, the cause of a recessive hereditary disease known as Familial Mediterranean Fever (FMF). This gene mutation results in abnormal functioning of pyrin protein that controls inflammation. The exacerbated inflammatory process becomes prolonged and inappropriate, damaging major organs.
FMF occurs around the Mediterranean and includes people of Armenian, Arab, Turkish, and non-Ashkenazi Jewish descent. Unfortunately, these recessive conditions are transmitted when two carriers parent children, as in cousin-marriage for example.
There were and remain a few in my family on both sides who suffer similarly to me; some died suddenly in their fifties of heart attack, stroke, or renal failure, three of my grandparents among them. They left widows to care for a large number of children in South Africa, far from their families in Lebanon; my father and his two sisters went into the Nazareth Nuns’ orphanage for seven years. (1922-1929).

Heart disease was accepted as a killer in those days. Early deaths were blamed on ignorance about lifestyle: lack of exercise, smoking, alcohol consumption, and “too much rich food,” as my maternal grandfather’s doctor told the family after my grandfather had fallen dead from a sudden heart attack.
A few of my Haddad-Yazbek female ancestors lived, like old growth trees in the forest, well into old age. We younger ones took refuge in their shade, listening to the stories of their deceased peers who, if they’d survived, may have told us their own versions firsthand.
The Past is Present
Cousin-marriage, common in some cultures, ignores the realities of heredity and its deleterious effects on children. Some grow into adults with life-threatening illnesses like my own.
Doctors warn against the practice. My firstborn died at birth with anencephaly, a neural tube defect, which may have been caused by active inflammation at a critical period of my pregnancy. In the twenty-first century, medical science has advanced to the point where diagnoses can retrospectively point to the ancestral origins of genetically transmitted diseases.
“Genetics loads the gun, environment pulls the trigger.”
Genetics loads the gun, environment pulls the trigger. It is vital to know what underlying conditions I carry for the safe management of my symptoms, even if there is no cure, and for my descendants who may battle unknowns in their own medical profiles.
The question of whether to publicly divulge one’s genetic status can be vexing. Our world is yet to formulate protocols for dealing with, for example, prospective employees who are asked to disclose their health status. Families can view revelations of heredity as a threat to those who suffer and are not diagnosed, or others who hide in shame, or are fearful based on their parents’ history.
I have deep admiration and respect for my parents and theirs who battled, with faith and stoicism, similar pain and fevers that beset me. It opens my eyes to why my parents were so forcefully positive in life, with denial and avoidance of anything troubling. Having lost their parents in early childhood, an unspoken disquiet underpinned the fight to overcome the travails in their bodies.
Knowing my genetic profile and its risks, I try to live safely. My immunologist suggested that my vegan Mediterranean diet, based on traditional Lebanese recipes as taught to me by my mother and her mother (yes, even shish barak can be vegan), and daily life with yoga may be keeping me alive and in reasonable shape at seventy.
As a writer of my Lebanese family history, I am contacted by readers of Lebanese origin asking me about their family history, their ancestors long gone. Sometimes they feel lost, rootless, even depressed. A conception of our origins, including our family medical history, is part of our inner constellation for good health, giving us a view of our ancestors that feeds our souls.
Further Reading on Familial Mediterranean Fever:
Ben-Chetrit, Eldad and Micha Levy. “Familial Mediterranean Fever.” The Lancet, vol. 351 (1998): 659–664.
Life at a Tangent with Familial Mediterranean Fever by Cecile Yazbek (unpublished)
- Categories: